Autonomic NS plasticity after spinal cord injury
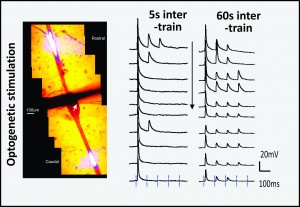
The injured spinal cord often becomes hyper-responsive resulting in autonomic dysfunction and devastating chronic pain syndromes. Spinal preganglionic sympathetic neurons are the sympathetic output neurons of the CNS and are located in thoracic and upper lumbar spinal segments. Loss of brain controls to SPNs after spinal injury leads to an unregulated circuitry strongly influenced by afferent input from pain systems, which can produce autonomic dysreflexia.
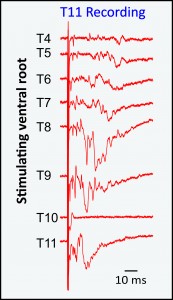
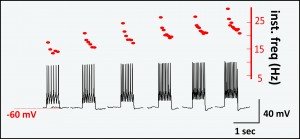
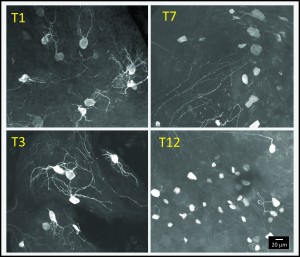
Sympathetic postganglionic neurons (SPNs) represent the final common sympathetic motor output. Thoracic SPNs (tSPNs) located in paravertebral chain ganglia receive convergent input from preganglionic neurons, providing the dominant sympathetic control of vascular function in the trunk and upper extremities. Given their strategic nodal site in autonomic signaling to body, any plasticity in tSPNs is likely to be of high significance. Yet tSPNs are inaccessible for in vivo study, so operational principles are inferred from studies in cervical and lumbar chain ganglia. To date, only a few in vitro studies have revealed tSPN electrophysiological properties, and there are still no accurate recordings of their cellular integrative properties or underlying recruitment principles.